Abstract
Per WHO 2016 and 2022 (5th ed.) myeloproliferative disease guidelines, Chronic Myeloid Leukemia (CML) is classified under two major groups according to the presence of bcr-abl translocation; these groups require different treatment approaches and show clinical presentation heterogeneity. Treatment agents such as tyrosine kinase inhibitors (Imatinib, Dasatinib, Nilotinib, Bosutinib, Ponatinib, Radotinib), Omacetaxine and Asciminib have been used in the treatment of Bcr abl positive CML according to the patient's clinic and mutation status. According to the IRIS study, a study evaluating CML patients treatment response to imatinib, the major molecular response was 33.3% at 3 months, the major molecular response was 48% at 6 months, and the major molecular response was 62.1% at 12 months; furthermore, the rate of achieving a complete molecular response at 12 months was 94.9% (4). In patients who was treated with imatinib as first line therapy, the rate of transformation to accelerated or blastic phase at 18 months was 0.9% in the MMR group and 9.9% in the non-MMR group. In "conventional" CML patients, high leukocyte counts may be accompanied by thrombocytosis; though presentation with only thrombocytosis without leukocytosis is hardly described so far. In this poster presentation, we introduced 7 cases who initially presented with isolated thrombocytosis and then diagnosed with Ph(+) CML.
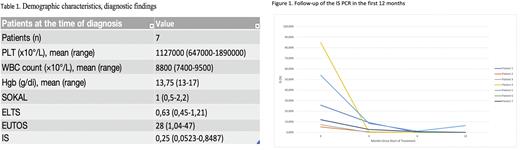
This study was conducted in three adult hematology centers from Antalya, Izmir and Istanbul. 400 patients followed in these centers were reviewed retrospectively; seven patients presented with isolated thrombocytosis were identified. Demographic characteristics, diagnostic findings, and risk scores of these patients were evaluated (Tablo 1). Eln 2013 response criteria were used for evaluation of response for 3rd, 6th, 12th. monthly responses (Figure 1).
Here we present 7 CML patients without leukocytosis who were diagnosed with marked thrombocytosis. The patients had similar symptoms and physical examination with no obvious splenomegaly or thrombosis. All of the patients had minimal basophilia and normal peripheral smear findings. All patients responded well to imatinib therapy. During follow up patients who maintained their MMR achieve had a better clinical course and prognosis compared to other CML patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal